Behavioral telehealth is transforming the way rural communities navigate mental healthcare challenges. There are many immediate benefits of telehealth that result in expanding access and improving the quality of care.
How telehealth improves access to care in rural communities
Telehealth allows small rural hospitals and clinics to provide quality healthcare services locally and at lower costs. This benefits rural patients since they are no longer required to travel long distances to access specialty care. Avoiding patient transfers is critical for both small hospitals and provider viability in rural areas. It also helps tertiary care centers keep beds open for patients in need of critical care.
Using telehealth to provide specialty services is more feasible for rural healthcare facilities than staffing those facilities with specialty providers. Telehealth makes a wider range of healthcare services available to rural communities via telemedicine, including:
- Psychiatry and behavioral health services
- Medication for Opioid Use Disorder
- Ophthalmology
- Dermatology
- Dentistry
- Audiology
- Cardiology
Effective telehealthcare services and programs in rural communities
- Chronic care management interventions provide patients with access to integrated care during their primary care visits.
- Provider-to-provider models allow rural primary care providers and specialist providers to work as a team to share knowledge and manage patient care. E-Consults are an asynchronous provider-to-provider model.
- Access to emergency care providers in real-time for evaluations and consults with local providers.
- Home monitoring can engage patients in their homes between medical visits by helping them effectively manage their conditions. Bridges to Care Transitions-Remote Home Monitoring and Chronic Disease Self-Management is an example of a telehealth remote monitoring program that assists patients with behavioral health conditions in their homes.
- Long-term care services offered through telehealth can bring specialized care to elderly populations who reside in long-term care facilities.
- Online therapy and remote counseling link rural residents with urban behavioral health and mental health counseling services.
- Telepharmacy extends access to pharmacy services, including medications and medication counseling, at rural healthcare facilities and community pharmacies.
- Interpreter services can be transmitted on-demand through audio and/or visual technology for patients who speak limited or no English.
Programs supported by telehealth offer new methods for improving healthcare access and quality by extending the reach of healthcare services, improving the ability of rural providers to address a broader range of medical conditions, and facilitating collaboration between professionals with limited access to their colleagues. Provider Bridge is a platform that connects healthcare providers with state agencies and healthcare organizations to increase patient access to telehealth. The National Emergency Tele-Critical Care Network (NETCCN) is another collaborative resource project that has emerged as a result of the COVID-19 pandemic, providing surge support by virtually connecting providers to a clinical-technical team trained in critical care assistance.
Challenges of telehealth in rural communities
Despite the promise telehealth holds for improving access to healthcare services in rural areas, there are policy barriers and infrastructure inadequacies that must be overcome.
Insurance Reimbursement
The issue of Medicare reimbursement is commonly cited as a major challenge for telehealth programs, including concerns related to geographic and originating site restrictions, provider restrictions, and service restrictions.
Individual state Medicaid programs vary in their guidelines regarding reimbursement for telehealth services. The 2019 National Rural Health Association (NRHA) policy brief Telehealth in Rural America elaborates on barriers to telehealth and provides policy recommendations to increase access to telehealth. Reimbursement by private payers for telehealth services can also vary. Some health insurance companies reimburse for telehealth services, while others do not.
In response to the COVID-19 pandemic, the U.S. Department of Health and Human Services implemented temporary policy changes to increase flexibility in offering telehealth services, including reimbursement. These changes address many of the barriers described above, but those barriers may return if changes in telehealth policy are rescinded after the public health emergency ends.
Licensure
The 2013 NRHA policy brief, Streamlining Telemedicine Licensure to Improve Rural America, describes how the current physician and therapist licensure system places burdens on physicians wanting to expand their practice to rural areas. Physicians who wish to practice across state lines must be licensed by the professional licensing board in each state where they are delivering care to patients. Actions states have taken to ease licensure barriers and the associated burden are:
- Offering specific licenses for telehealth
- Reciprocity and endorsement with other states
- Creating interstate compacts
In 2021, the Federation of State Medical Boards, with the support of HRSA and HHS, launched Provider Bridge, a platform that facilitates license portability to allow providers to submit credentials and treat patients in high-demand areas via telehealth. Supporting licensure compacts helps to expedite the process for qualified service providers to be licensed to practice in multiple states.
Broadband
Affordable broadband is required to support telehealth programs, health information technology, and health information exchanges, all of which increase access to and the quality of healthcare. Traditionally, healthcare facilities needed broadband to provide telehealth services, but with modern applications of telehealth such as remote patient monitoring and e-visits, broadband is also necessary in patients’ homes. Many rural communities do not currently have access to internet connection speeds that support efficient transmission of data to provide telehealth services. The broadband gap has the potential to lead to a new set of health inequities due to disparate access to telehealth. The 2021 report Broadband Today: Rural America’s Critical Connection discusses the importance of broadband access to rural business, telehealth, and remote work opportunities.
Stigma
Nearly 1 in 5 adults in the U.S. experiences a mental disorder within any given year according to the National Alliance on Mental Illness. Yet, the misconceptions, myths, and cultural stigma associated with mental illness are significant barriers that keep people with mental health disorders from seeking and receiving treatment in rural areas. Factors that may influence rural residents to avoid seeking care include such issues as:
- Lack of understanding and knowledge of mental illness, including among healthcare staff
- Prejudice or stigma towards mental illness treatment
- Secrecy about mental illness in the community and general hesitancy to seek care
- Perception of a lack of confidentiality and privacy in small towns with closely-tied social networks
While there are drawbacks to living in small communities when it comes to mental health, small communities have clear strengths and can create a strong foundation of mental assets for their populations as well. The close-knit nature of rural communities can mean that residents are more likely to rally around each other and provide community support in times of need. A strong external support group can help facilitate a person’s success in treatment and also help support the family’s efforts in attending to the care seeker.
Suicide: a rising rural mental health concern
Suicide continues to be higher in rural counties, and the gap between rural and urban suicides has widened over time. A 2017 CDC report, Trends in Suicide by Level of Urbanization — United States, 1999–2015, discusses possible causes for the geographic disparity:
- Limited access to mental healthcare
- Social isolation
- The opioid overdose epidemic
- Economic recession
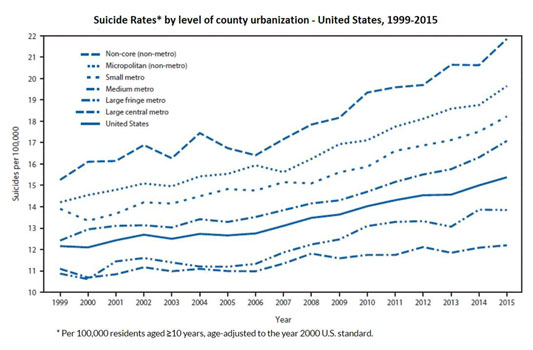
According to a 2020 report from the CDC, from 2000 to 2018, the rural suicide rate increased by 48%, while urban rates increased by 34%. In 2018, the suicide rate in rural counties was 19.4 deaths per 100,000 compared with urban counties at 13.4 deaths per 100,000.
Additional information regarding the impact of suicide in rural communities can be found in Understanding the Impact of Suicide in Rural America.
Impact of telehealth on rural healthcare providers
Telehealth use in unpopulated rural areas can reduce a provider’s feelings of isolation and burn-out and subsequently improve provider retention. Telemedicine: Changing the Landscape of Rural Physician Practice highlights testimonials from healthcare providers practicing in rural areas throughout the U.S.
Healthcare systems with the infrastructure and staffing to support telehealth services impact how rural providers are able to provide patient care by giving them access to:
- Team-based care
- Other specialists and subspecialists for consults in real-time
- Virtual networks with peers
- Outsourced diagnostic analyses
- In-home monitoring of patients for follow-up care
- Continuing education and training, reducing travel and out-of-practice time
Financial impact of telehealth on rural facilities and communities
The financial impact of implementing telehealth services in a community can vary, depending on the type of healthcare service or services to be offered using telehealth and the patient population. Anticipating Economic Returns of Rural Telehealth, a 2017 NTCA—The Rural Broadband Association report, describes telehealth potential benefits, including the following quantifiable benefits:
- Decreased transportation costs
- Minimizing lost wages
- Reduced hospital staffing costs
- Increased local lab and pharmacy profits
The report also lists nonquantifiable benefits:
- Increased access to specialists
- Providing timely care
- Ensuring patient comfort
- Reducing the need for transportation
- Benefits to the provider
- Improved patient outcomes
Antelope Recovery Aims to Provide Accessible Care for All Rural Colorado Communities
At Antelope Recovery, we are committed to breaking down barriers to treatment and ensuring that quality mental health care is within reach for all rural Colorado residents. Our telehealth programs are designed to bridge the gap, offering convenient and effective solutions for individuals and families in remote areas. We believe that everyone deserves access to the support they need, regardless of their location. If you’re a rural provider or a resident seeking reliable telehealth services, consider Antelope Recovery as your partner in promoting mental health and well-being. Together, we can create a brighter, healthier future for all rural communities in Colorado.


